Abstract
Introduction: Sickle cell anemia (SCA) is the most common genetic disease identified in newborns in the United States, and pulmonary complications are the second most common cause of hospital admissions. Children with SCA commonly experience impaired growth, delayed puberty, elevated metabolic rate and increased protein turnover. These factors may contribute to a decreased body weight, specifically fat-free mass, despite seemingly adequate caloric intake. Multiple studies have reported significantly lower body mass index (BMI) in children with SCA, compared to age-matched children without SCA.
In children with cystic fibrosis, there is a well-established relationship between low BMI, malnutrition, and a decline in lung function. A normal body weight has been associated with a slower decline in pulmonary function and a decrease in mortality. Pulmonary cachexia syndrome is a distinct phenomenon in adults with chronic lung disease defined as a disproportionate cytokine driven loss of skeletal muscle. Patients frequently have low BMI (<20kg/m2), low fat-free body mass, with a normal caloric intake. Pulmonary cachexia has been most prominently studied in the chronic obstructive pulmonary disease (COPD) population. Although children and adults with SCA can develop chronic lung disease, pulmonary cachexia syndrome and the impact of nutritional status on pulmonary function has yet to be defined in this population. Lung function decreases with age in the sickle cell population and FEV1% predicted < 80% has been found to be associated with early death in adults with SCA.As children with SCA in the US survive into adulthood, nutritional status may be a contributing factor in chronic lung disease. In a prospective longitudinal multi-center cohort study of children with SCA we hypothesize that a lower BMI is associated with a significant decline in FEV1% predicted over time.
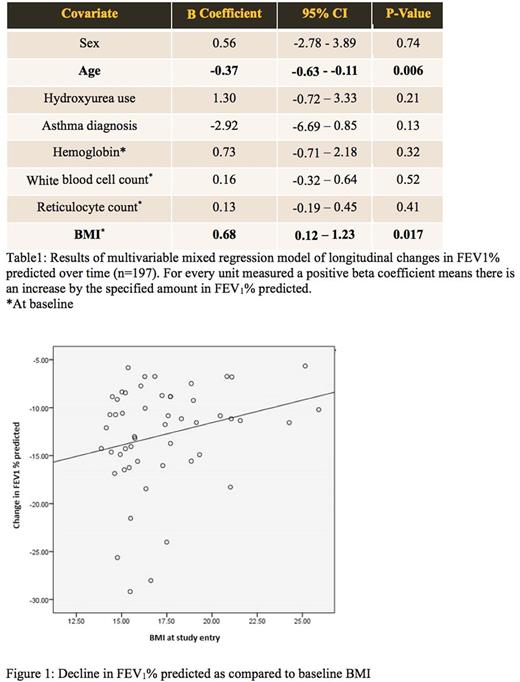
Methods: In the NIH sponsored prospective, multicenter, Sleep and Asthma Cohort (SAC) study, children with SCA, defined as HbSS or HbSβ°, unselected for respiratory disease, were enrolled from 3 large clinical centers. Study certified pulmonary function technicians performed spirometry with central review. Participants had a minimum of 3 spirometry measurements performed at least 12 months apart (mean 4.4. years apart). Predicted values were determined for FEV1 based on the Global Lung Index (GLI) 2012 multi-ethnic reference equations. Height and weight were used to calculate BMI at study entry. In a multivariable model, the following independent covariates were used to predict a longitudinal change in FEV1 % predicted: baseline BMI, sex, history of asthma (defined as a physician diagnosis as well as the use of either inhaled corticosteroids or bronchodilator), baseline labs such as hemoglobin, reticulocyte count, white blood cell count, and the use of hydroxyurea at any point in the study period.
Results: A total of 197 participants with SCA between the ages of 6 -19.3 years (mean age of 11) were included in the analysis. Mean BMI of the cohort at study entry was 16.9 kg/m2. Participants were followed over a range of 1.1 - 6.5 years from baseline to endpoint. In a multivariable model, for every one unit increase in BMI there was an increase in FEV1 % predicted of 0.68% (P=0.017). FEV1 % predicted declined by 0.4% for every additional year of age (p=0.020). Sex, asthma history, hemoglobin, reticulocyte count, white blood cell count, and hydroxyurea therapy were not significantly associated with a decline in FEV1 % predicted over time. The two significant risk factors for a decrease in FEV1 % predicted over time were increasing age and decreased BMI at baseline.
Conclusions: In a large prospective cohort study of an unselected group of children with SCA, low baseline BMI is associated with a more significant decline in FEV1% predicted over time. Longer prospective studies are needed to determine if the decline in FEV1% predicted is reversible with disease modifying therapy and nutritional modifications.
Rodeghier: Rodeghier consultants: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal